This week we explore a rare case report of phentermine-related tardive dyskinesia, the quest to find neural markers in someone who’s attempted suicide, and a letter to the editor arguing for greater awareness of the link between maternal mental health and fetal interventions.
Case Study Highlights Rare Case of Phentermine-Related Tardive Dyskinesia
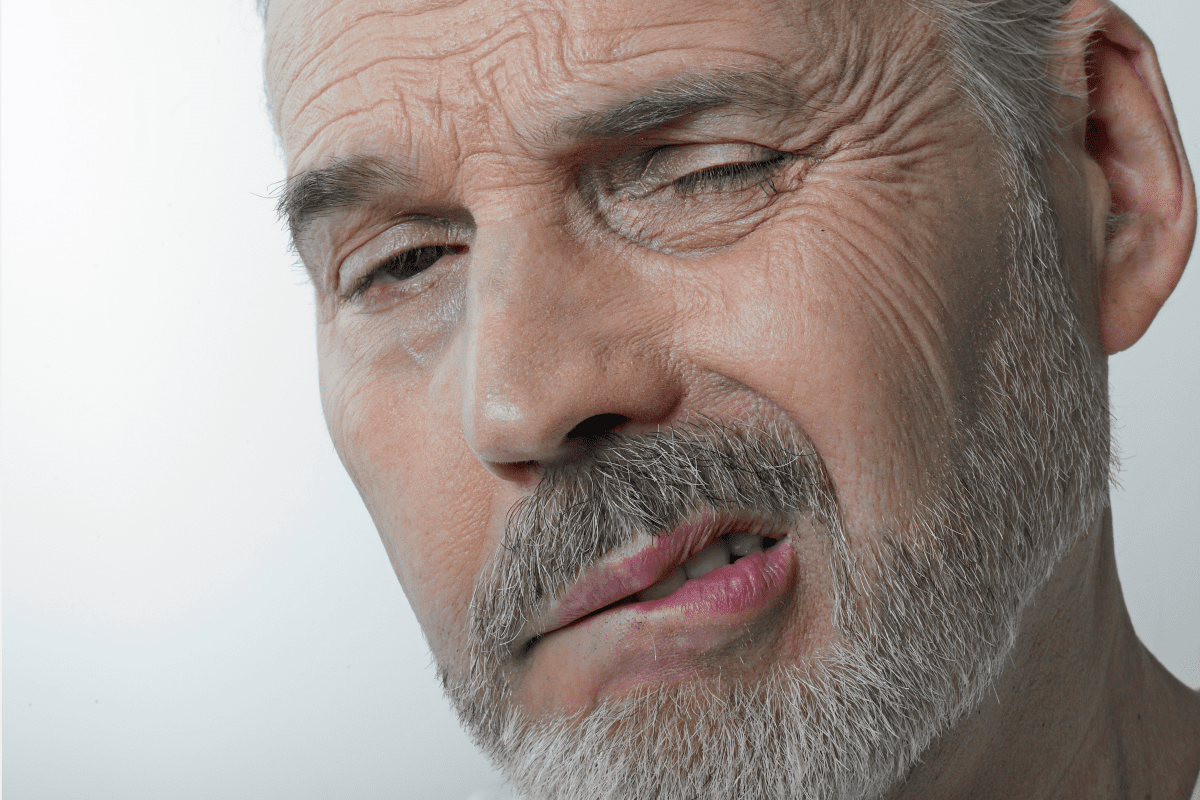
Tardive dyskinesia, a condition marked by persistent, repetitive involuntary movements, that typically affect the face, tongue, and lips, normally occurs as a result of prolonged use of antipsychotics or other dopamine receptor antagonists.
The typical risk factors include advanced age, gender (women suffer more frequently), extended antipsychotic use, prior movement disorders, organic brain dysfunction, alcohol abuse, and specific genetic markers.
A recent case report, appearing in The Primary Care Companion for CNS Disorders, details a 79-year-old woman who developed tardive dyskinesia after taking phentermine to treat low energy and weight control. With a medical history including major depressive disorder and generalized anxiety disorder, she was already on a regimen of desvenlafaxine, buspirone, hydroxyzine, and lorazepam.
In April 2023, her caregivers prescribed atomoxetine. But because of fluctuating mood and energy levels, she switched to phentermine in August 2023. A month later, she developed involuntary facial movements. Her doctor immediately pulled the phentermine and reintroduced atomoxetine. Her symptoms resolved by October.
Phentermine acts by increasing norepinephrine and epinephrine secretion. But it also comes with a broad spectrum of side effects. Even so, there are few documented reports of phentermine-induced dyskinesia.
Unlike amphetamines, phentermine minimally affects dopamine release. Even so, we still don’t fully comprehend its precise impact on dopamine. A phase IV study reported tardive dyskinesia in 0.13% of 14,395 phentermine users, highlighting the potential, though rare, risk of tardive syndromes with stimulant use. This case represents the third documented instance linking phentermine to tardive dyskinesia.
The authors argue that more research investigating the development of movement disorders related to phentermine, despite the rarity of such side effects, is imperative given how much it can impair social functioning. Recognizing the potential for phentermine-induced tardive dyskinesia remains critical for appropriate patient monitoring and management.
IN OTHER PSYCHIATRY AND NEUROLOGY NEWS
- The Journal of Clinical Psychiatry published research this week that sought to identify neural markers of suicide attempts using resting-state functional magnetic resonance imaging.
- PCC also published a systematic review evaluating the effects of a ketogenic diet on epilepsy in children and adolescents.
- In a letter to the editor of JCP, the authors offer guidance and hope to raise awareness about the intersection of maternal mental health and fetal interventions.
- Another case report in PCC discusses the utilization of a three-times-daily prazosin dosing scheme during hospital admission for a patient experiencing severe nightmares and daytime flashbacks associated with PTSD.
- Finally, recent research highlights the importance of monitoring sleep patterns when looking out for – and treating – suicidal ideation.