Traumatic brain injuries (TBIs) remain an all-too-common part of life, with annual incidences numbering anywhere between 27 and 69 million in the United States. Research shows that falls, car accidents, and assaults are responsible for most TBIs, but sports-related injuries – primarily among kids and young adults – are on the rise.
Healthcare providers look for a range of symptoms when making a diagnosis:
- Physical issues such as headaches, dizziness, and seizures.
- Cognitive impairments in memory and attention.
- Neuropsychiatric problems, including anxiety, depression, and PTSD.
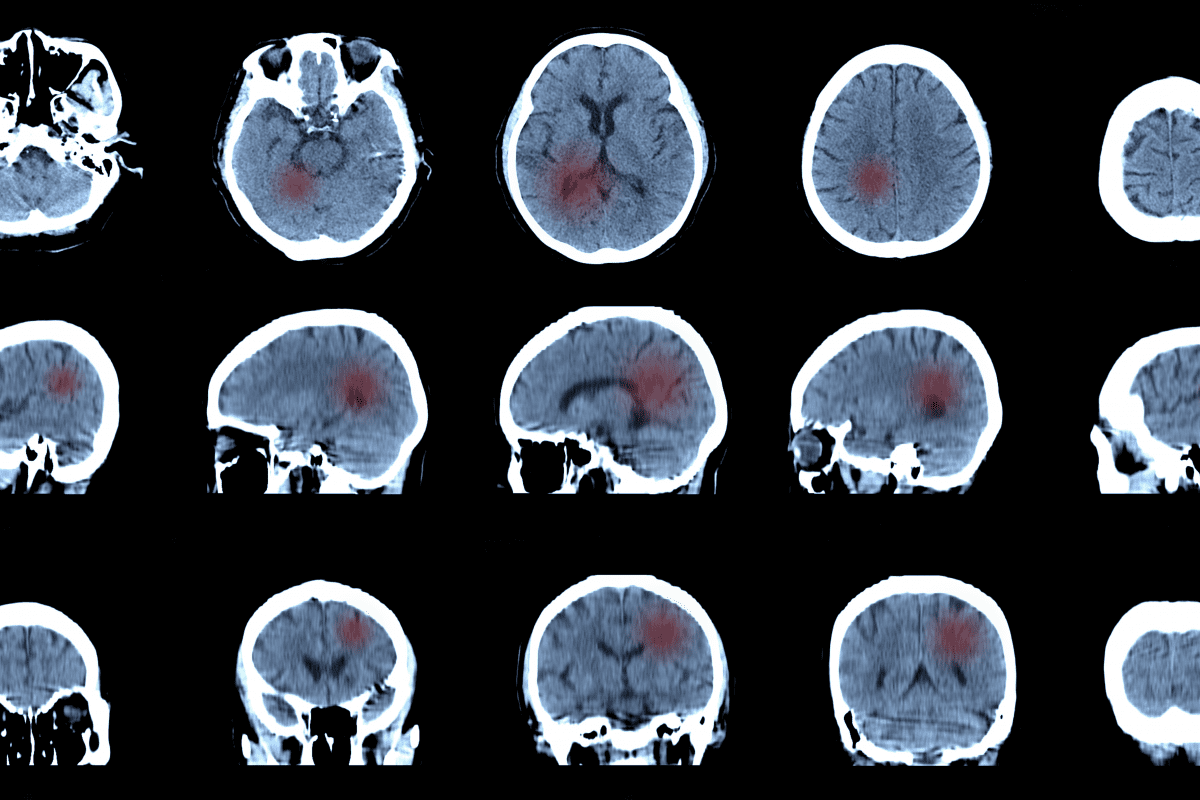
Additionally, doctors rely on neuroimaging techniques like CTa and MRIa to track down structural damage, while advanced methods like DTI and PET provide insights into microstructural changes and brain metabolism. Cognitive testing, including neuropsychological assessments, helps evaluate the extent of cognitive deficits and guides treatment planning.
TBI management demands a multidisciplinary approach. Rehabilitation can involve physical, occupational, and speech therapy to address motor and cognitive impairments. Mental health support is crucial, too, since so many cases include psychiatric comorbidities. Effective treatments include psychotherapy, medications for depression and PTSD, and complementary therapies like acupuncture and mindfulness.
The Primary Care Companion for CNS Disorders has published a wealth of research that helps caregivers diagnose and treat TBI cases. This week, we’re presenting summaries of three of the more recent studies – with links – for further review.
Shift in Care Approach Transforms Recovery for Veterans with TBI
TBIs pose significant challenges for patients and providers alike. A new case study in Primary Care Companion for CNS Disorders about Army Sgt. 1st Class Mr. B highlights these challenges and the effectiveness of a multifaceted treatment strategy.
Mr. B, a 15-year veteran, sustained a mild TBI (mTBI) and a left lower extremity amputation following an IED blast injury in Afghanistan. After medical personnel declared him “stable” overseas following treatment – along with subsequent care at a U.S. military hospital – a range of new symptoms cropped up. These included severe irritability, poor sleep, and significant pain. The sergeant’s excessive alcohol use – which he embraced as a coping mechanism – only made things worse.
Caregivers decided to tackle his alcohol dependency and sleep disturbances first. They prescribed him naltrexone and a CPAP machine for sleep apnea, leading to notable improvements in mood and pain management. This positive change fostered a better relationship with his PCP, which paved the way for a more comprehensive treatment plan.
Doctors overhauled Mr. B’s regiment, starting with the introduction of venlafaxine and gabapentin, which proved more effective for his pain and mood issues. Physical therapy, prosthetic adjustments, and dietary changes further enhanced his recovery. Maybe more importantly, he started – and stuck with – therapies such as cognitive processing and art and music therapy – which helped manage his traumatic experiences and cognitive impairments.
The case backs up the importance of a holistic and multidisciplinary approach to TBI treatment. By involving physical, psychological, and social support systems, Mr. B significantly improved functionality and quality of life. He resumed active duty, maintained his family relationships, and became a mentor to fellow soldiers facing similar challenges.
This case exemplifies how TBI patients, even those with mild injuries, might battle against persistent symptoms that necessitate comprehensive and tailored treatment plans.
While no FDA-approved pharmaceuticals specifically target postconcussive symptoms (yet), guidelines and a combination of therapies can help facilitate successful outcomes. Psychoeducation for patients and their families remains crucial, ensuring ongoing support and understanding of the condition’s complexities.
Case Study Highlights Clozapine’s Effectiveness in Treating TBI-Related Capgras Delusions
In another compelling case, a TBI patient developed Capgras delusions, convinced someone replaced his family with imposters. Despite hypersensitivity to multiple antipsychotic medications and no improvement, a switch to low-dose clozapine resulted in the complete remission of his delusions, highlighting a potential new treatment path for complex organic psychoses.
A 24-year-old Kuwaiti man, a former police officer with no prior neuropsychiatric history, began experiencing paranoid delusions three months before his admission.
As it turned out, he’d suffered a severe TBI in a car accident a year earlier. This led to a loss of consciousness, seizures, and an extended ICU stay. He managed to do OK after the accident, aside from minor headaches and problems concentrating. He then developed Capgras delusions. The Capgras delusions instilled panic, disrupted his sleep, and eventually led to social withdrawal.
Initially treated at a private psychiatric facility, doctors diagnosed him with psychotic depression. They prescribed escitalopram, aripiprazole, and clonazepam. But severe side effects, such as akathisia and torticollis, forced doctors to tweak his medications multiple times without success. Eventually, they admitted him to an inpatient facility.
Comprehensive evaluations, including lab tests, toxic screens, and neuroimaging, all appeared normal. Neuropsychological assessments revealed slow processing speed and attention issues. Caregivers then pivoted to clozapine, starting at 12.5 mg daily and increasing it to 150 mg daily over two weeks. Remarkably, his delusions faded away without significant side effects.
Capgras syndrome involves delusional misidentification, commonly seen in schizophrenia, mood disorders, and brain injuries. The doctors theorized that it stems from a disconnect between the brain regions responsible for facial recognition and emotional processing.
Psychotic symptoms can emerge early or late after TBI, often complicating treatment because of how sensitive most patients are to antipsychotics. Clozapine, known for its effectiveness in refractory psychosis, demonstrated an impressive response in this case, despite its normally intimidating side effects.
Study Links TBI in Service Members to Unsafe Firearm Storage Practices
It’s a quiet crisis. Suicide is skyrocketing among veterans, most of which – 60% to 70% – involve firearms. TBIs play an outsized role among this population. A startling 97% of TBI-related suicides from 2000 to 2017 involved firearms, according to the U.S. Centers for Disease Control and Prevention. Clear explanations remain elusive and generally unsafe storage practices among TBI patients don’t help, which led to this final research paper.
The study involved 378 firearm-owning National Guard personnel, mostly men (91%) and white (74.6%), with an average age of 27.4 years. Researchers recruited the participants from a joint forces training center in the southern United States. The researchers analyzed TBI data using the Traumatic Brain Injury-4 (TBI-4) self-report measure, which identifies suspected TBIs based on loss of consciousness.
Additionally, the researchers outlined three types of firearm storage practices:
- Unsafe (loaded, non-secure location).
- Safe (unloaded, secure location).
- Mixed-secureness.
The researchers culled data from between November 2013 and June 2014.
The results?
- 27 percent of participants screened positive for a suspected TBI.
- And those with a suspected TBI were much more likely to store firearms unsafely – 26.5 percent vs. 14.9 percent.
- And they were less likely to store them safely – 35.3 percent vs. 48.9 percent.
In short, researchers linked the severity of TBIs to unsafe storage practices. And the team found no notable differences in mixed-secureness based on TBI status or severity.
The paper’s authors suggest that some typical neuropsychiatric issues after a TBI, such as impaired executive functioning and impulsivity, might hinder safe storage practices. They also pointed to other factors, such as psychiatric comorbidities (e.g., PTSD) and sociodemographic variables that might play a role.
Further Reading
Weekly Mind Reader: Using Video to Curb Stigma of Mental Illness