Between 16 and 50 percent of patients on antipsychotics ultimately develop the involuntary movement disorder known as tardive dyskinesia (TD).
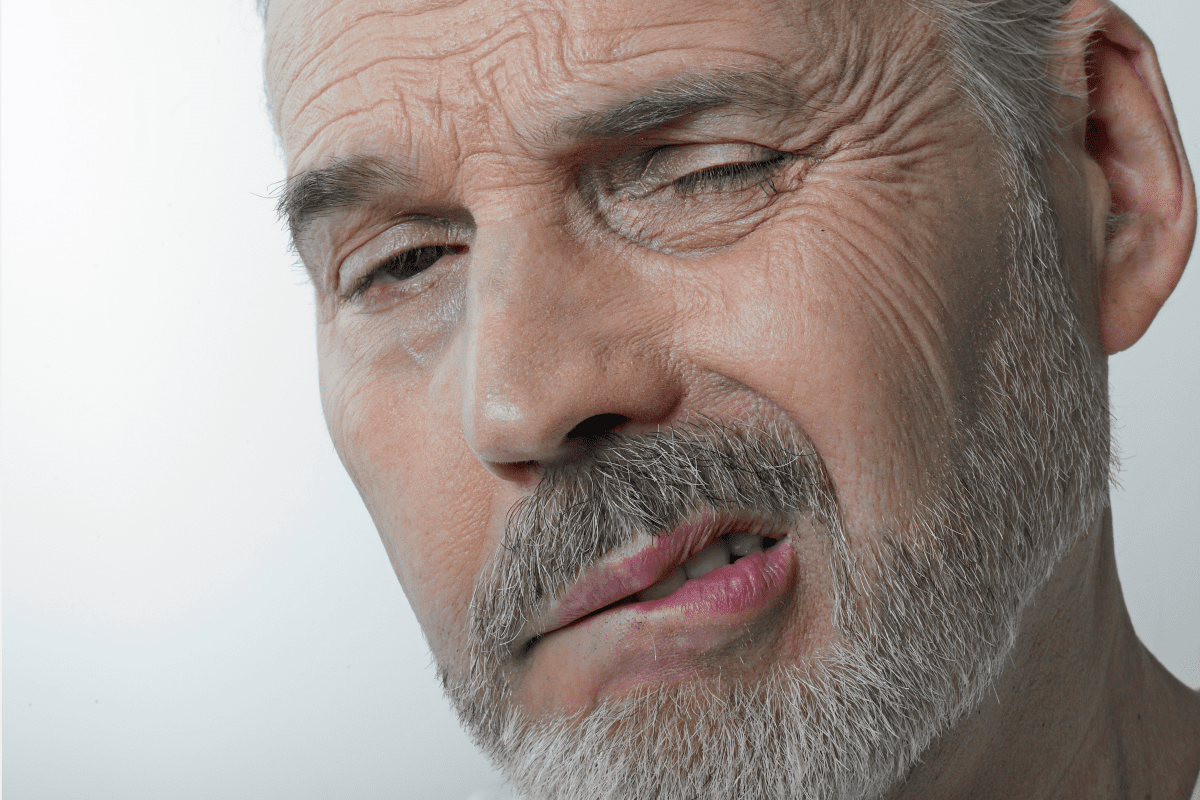
Scientists aren’t entirely sure what causes the uncontrollable jerkiness and grimacing associated with TD. They strongly suspect that the antipsychotics–typically prescribed to treat schizophrenia, bipolar disorder and depressive disorders–block the dopamine receptors in the brain to create a state of “dopamine supersensitivity” that sets off the abnormal movements. Risk increases with the duration of treatment and the use of first-generation antipsychotics versus the newer atypical antipsychotics.
Tardive Dyskinesia and LAI Antipsychotics
Prevalence of Tardive Dyskinesia in Medical Records
Diagnostic and Treatment Fundamentals for Tardive Dyskinesia
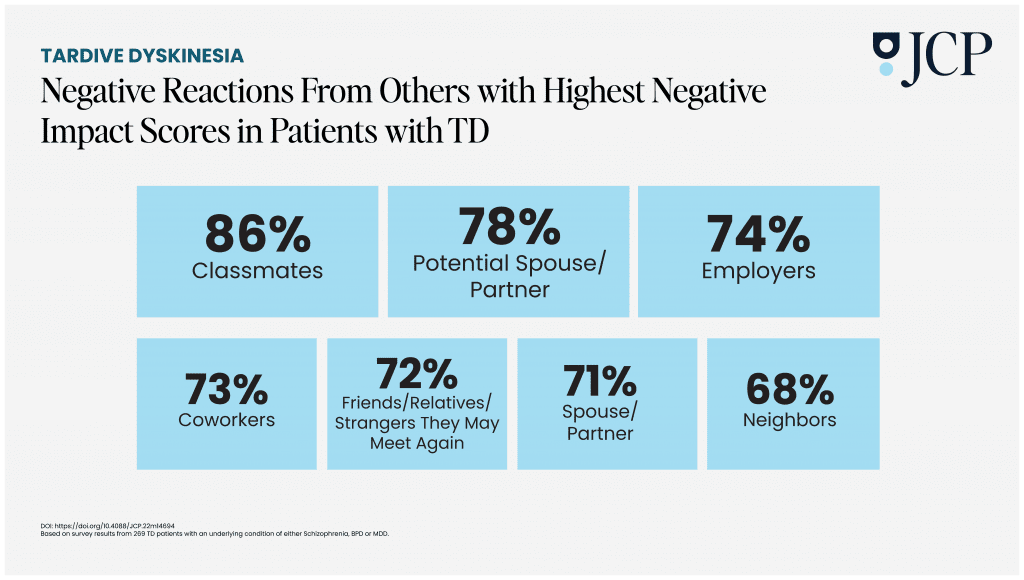
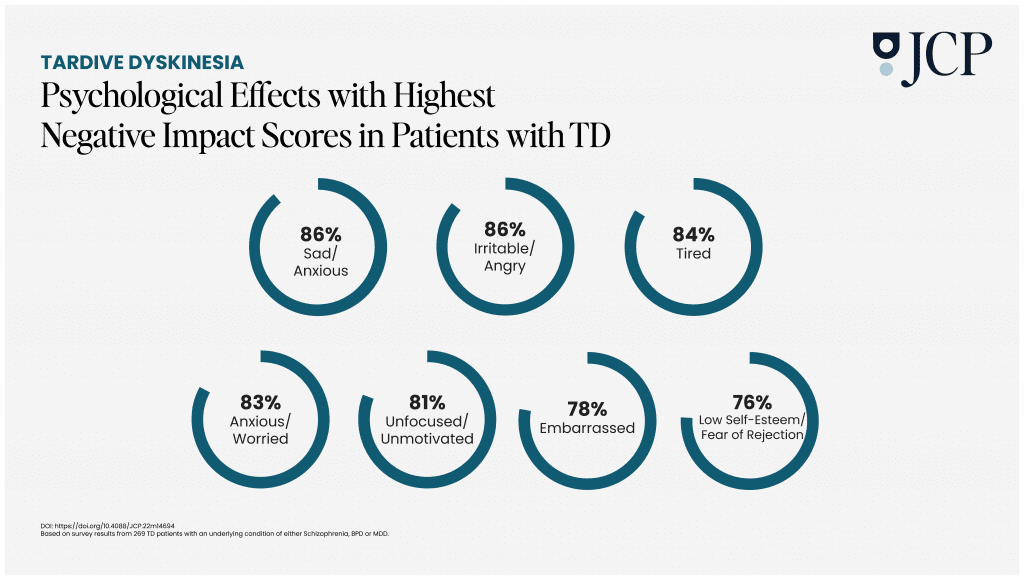
Recently, nine health care professionals with expertise in TD and clinical scale development met to discuss how to measure the negative outcomes of the condition on the lives of patients, and published the results in The Journal of Clinical Psychiatry.
Understanding TD Symptoms
“For some patients, even very mild movements may cause quite a dramatic impact. And for some patients, even more severe movements don’t impact their day to day life. We wanted to give them–and their caretakers–a way to judge,” said Richard Jackson, MD, one of the lead authors of the paper.
Jackson, who is the director of research and the co-owner of the Neurobehavioral Medicine Group in Bloomfield Hills, Michigan, was part of the committee that designed a new and improved “Impact-TD” scale. The tool assesses five specific functional domains that affect TD patients: physical, social, vocational, and psychological, and psychiatric.
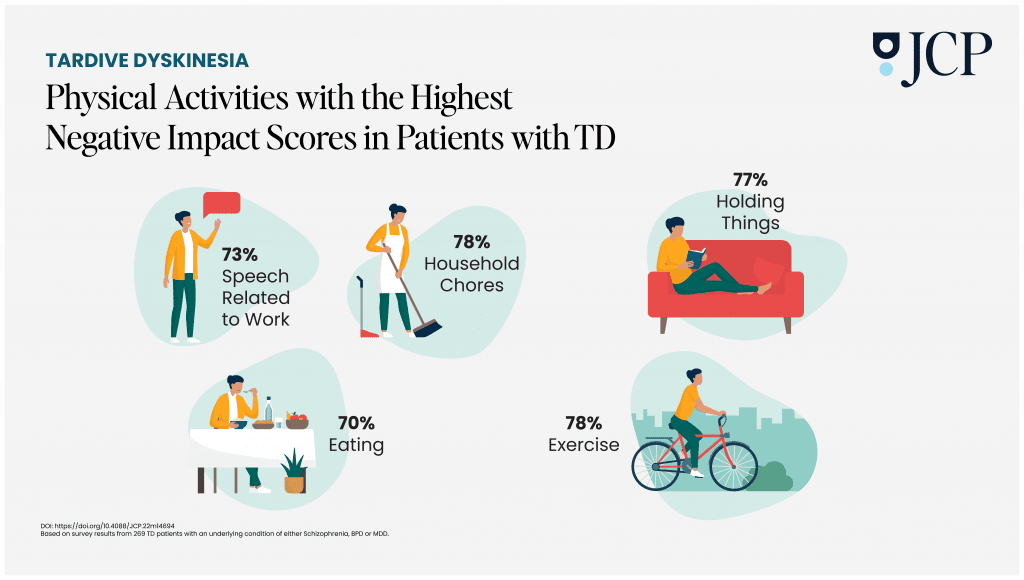
“Each patient characteristic was included for establishing specific, real-world examples where a patient might have difficulty functioning in daily life because of TD,” he explained.
Jackson said that this is the first standardized clinician-rated instrument that he is aware of designed specifically to understand the daily challenges of TD for each individual. He said he hoped it will enlighten clinicians on how subjective the experience of TD can be.
“You might have a guy that was playing chess and knocked over all the pieces and it was terribly embarrassing because no one even knew that he had mental illness. And that was most devastating to him. But you also may have someone with what you would consider severe symptoms and they say it doesn’t bother them,” he said.
The Development of Impact-TD Scale
Older TD scales only looked at the severity of the movements without considering the repercussions on a patient’s ability to function, Jackson said. They considered the severity of the movements but not necessarily the patient’s level of awareness and distress.
“The functional effects are sometimes underappreciated or ignored,” he said.
Another advantage to the updated scale is that it factors in the observations of people close to the patient, as well as their medical team. This, Jackson hoped, will help healthcare professionals understand the best ways to support both patients and their caregivers.
“It’s important for doctors to consider how the symptoms of TD affect a patient and this includes taking into account feedback from family and caregivers who spend a lot of time with the patient,” he said. “They can provide insight about how symptoms vary from day to day. They’re often the best source of information about these fluctuations.”
TD can change a person’s life on so many levels so it’s important to manage the condition comprehensively. That’s another win for the updated scale. It’s easy to understand so the various healthcare professionals who have a hand in treatment can use it, Jackson said.
Making Treatment Calls
TD often doesn’t resolve even if a patient stops treatment for the underlying condition, Jackson warned. And, while it’s an unfortunate risk factor, the symptoms of the primary mental illness can be so much worse. Patients who develop TD often have to navigate a delicate balance of treatment decisions.
All this makes regular assessment of TD essential, Jackson said. “If you catch it early and address it, you have a better chance of managing it and lessening the severity.”
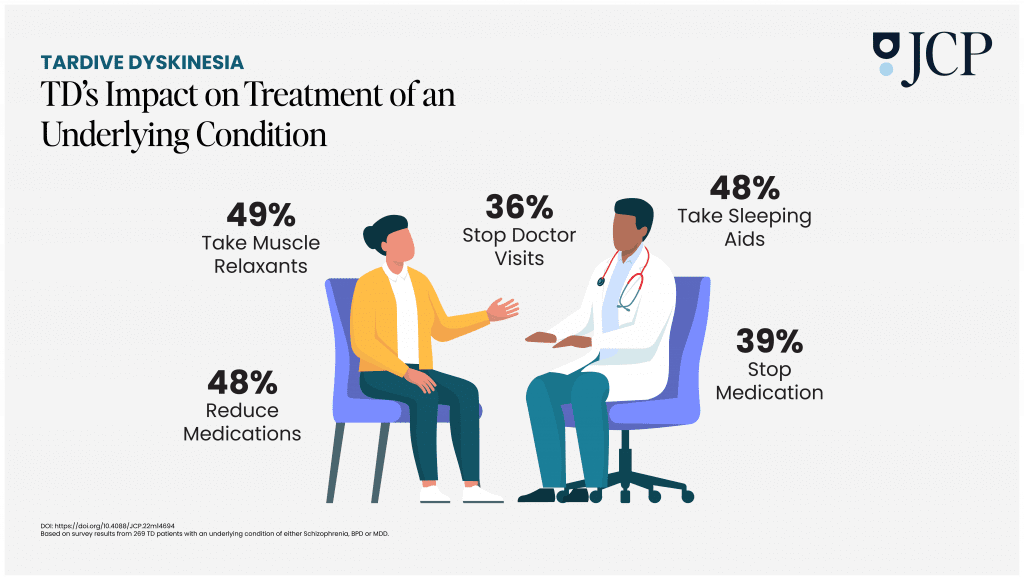
These findings were published in The Journal of Clinical Psychiatry. Read the full report here, as well as the survey results from another recent TD study from which the graphics in this report are based on.